It’s that time of year — not just for holiday cheer, for the flu
Everyone knows that the fall brings flu season, replete with aches, pains and a new version of the vaccine. But why is cold weather synonymous with this virus? Virologist and William & Mary Associate Professor of Biology Kurt Williamson recently talked with W&M News on the science behind this pathogen and hypotheses for why infections have a seasonal spike.
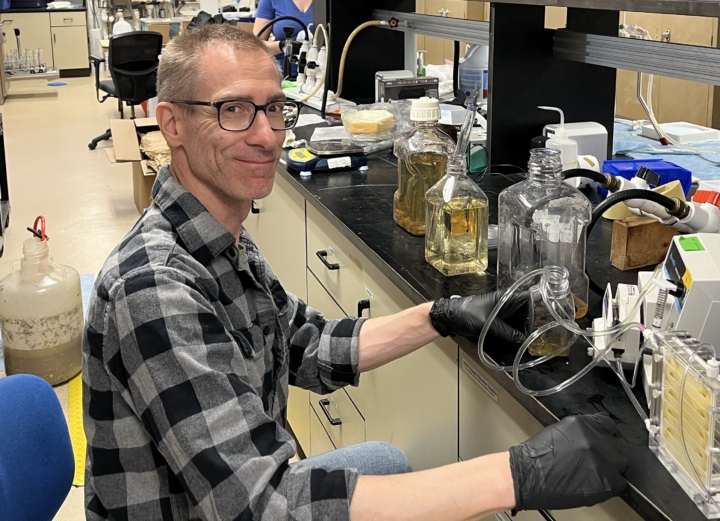
Williamson studies viromes, all the viruses in a given environment, to understand their role in essential ecosystem-level processes. A large portion of these viruses are classified as bacteriophages, viruses that infect bacteria. His lab is currently working on a Department of Agriculture-funded project looking at the viral and bacterial composition of soils managed under organic vs. conventional growing conditions.
The interview has been edited for length and clarity.
Q. How does one contract influenza?
A. Humans are social creatures, so you’ll typically contract the virus just by being in close contact with other people. The virus may get in through your nose or throat when you breathe the same air as an infected person. Touching a surface with live viral particles and then wiping your nose or rubbing your eyes can also do the trick. As a respiratory virus, influenza ultimately needs to get into your airways one way or another.
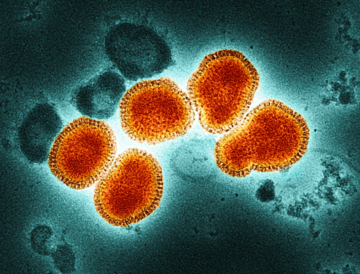
Q. And how exactly does the virus infect us once inside our bodies?
A. For a virus to infect us, our bodies must have a cell that has an appropriate receptor for the virus to bind to. It’s often described as a lock and key type relationship. There are actually many viruses we’re exposed to that don’t have the right key so they can’t infect us. But the flu can hook up with cellular receptors in our respiratory tract and fool them into thinking it’s cargo the cell needs for normal function. Then, kind of like a Trojan horse, the virus is ferried into the cell. Once inside the nucleus, the virus hijacks the cell’s machinery, and, not to anthropomorphize it too much, essentially convinces the cell that it needs to help the virus replicate.
Q. Where does the virus get its name?
A. It actually comes from an early misunderstanding of the disease. Bacteria were established as causative agents of disease about 200 years before viruses, so people initially thought that the sickness was caused by a bacterium called Haemophilus influenzae. Now we know the virus causes the initial infection. What can happen is you first catch the virus, which leaves you weak, and then you get a secondary bacterial infection which, worst-case scenario, leads to death. If you have a weakened immune system or preexisting health conditions, you really need to be careful.
Q. Why do we need a new flu shot each year?
A. The flu vaccine is reformulated to protect against the most widespread and virulent strains that have emerged over the past year. These new strains arise through two modes of mutation.
The first, called antigenic drift, results from small, gradual changes in the virus’ genetic code. When human cells replicate, they use an enzyme called DNA polymerase to build new DNA strands. A built-in proofreading mechanism follows behind, fixing any copying errors and keeping mistakes in our genetic code extremely rare.
The flu, on the other hand, stores its genetic material as RNA and uses an enzyme called RNA polymerase to copy viral RNA. But unlike DNA polymerase, RNA polymerase doesn’t have a proofreader. This makes copying errors — and therefore mutations — very common, roughly one per new virus.
Multiply that by the thousands of viruses produced by a single infected cell, the thousands of infected cells in a host and the millions of hosts in a population, and you get an astronomical number of mutated viruses. The mutations that perform the best are selected for and thus you get steady, gradual changes in the virus over time.
The second mutation method, antigenic shift, happens when two viruses infect the same host. Their genetic material gets mixed together, producing a completely new hybrid strain that’s potentially more pathogenic.
Q. Why does flu season happen in the late fall and winter?
A. There’s a bit of a backstory here. So, in 1992, British epidemiologist R. Edgar Hope-Simpson wrote a book called “The Transmission of Epidemic Influenza.” This publication challenged the classic understanding of how flu spreads in which one person infects another and so on, spreading the disease outward from one geographic point. But in examining flu outbreaks, Hope-Simpson found that this model of infection was inconsistent.
He noticed that the disease often peaked at nearly the same time in different locations. During the 1918 pandemic, for example, cases in U.S. cities including Boston, Philadelphia and San Francisco surged almost simultaneously. So he asked the question: If flu simply spreads person-to-person, how can epidemics synchronize across such distances?
Hope-Simpson hypothesized that flu viruses may persist in populations year-round, staying dormant until reactivation by some stimulus, even though there’s no known mechanism for this. His analyses pointed to sunlight — specifically, solar radiation — as a possible driver of these seasonal waves.
Unlike temperature, which can vary widely from city to city, sunlight changes predictably with latitude and season. Hope-Simpson observed peaks in the flu during the darkest months in each hemisphere — December to February in the north, June to August in the south — suggesting that sunlight may predict flu spikes. Sun exposure is positively correlated with immune system function. And the UV radiation from sunlight destroys viral particles, so in darker months, viruses survive longer in the environment.
But the solar radiation idea is just one hypothesis for the flu’s seasonality. The bottom line is, there are probably many different factors that contribute to this trend, and we’re not quite sure how they all work together or which contributes more.
The big question for a lot of virologists remains: Where is the virus when it’s not here? One challenge for flu is that it can be considered a zoonotic disease, meaning flu can be shared between humans, birds of different species, pigs and now cattle. So part of it could be that when flu’s not with us, it’s in some animal reservoir.
Q. You mention different factors like sunlight, that work to drive the seasonality of flu. What else might contribute to this?
A. Temperature does still play a role. Unlike our cells, which maintain balance through homeostasis, viruses have no way of responding to environmental stressors. Once a virus has left the host it can only last so long. Eventually it will fall apart, mostly through thermal decay. That degradation slows down in the cold, just like food lasts longer in your refrigerator.
Humidity is another factor. The warmer and muggier it is, think Williamsburg in July, the more water droplets clump together and fall out of the air, trapping the viruses in them and decreasing the chance you’ll breathe them in. Colder, drier air, like we typically have in the fall and winter, suspends viruses in the air longer.
The fall and winter are also holiday season. We’re spending more time gathered with family and friends indoors, which can increase transmission.
Q. What should you do if you get the flu?
A. Unfortunately, there aren’t many medicinal treatment options. The best way to protect yourself is proactively with the vaccine. If you get the flu, the best thing you can do is drink plenty of fluids and rest. Sleep really helps, allowing your body to devote more energy to your immune system. Not to get too nerdy, but it’s like when they’d divert energy in Star Trek to power up the protective shields; it’s a finite resource.
You should also try to eat nutritious food. Give your body the building blocks it needs to repair and replace the cells you’re losing.
Q. So … potato chips?
A. Well, a little bit of comfort food can’t do much harm.